Diabetic Retinopathy
Diabetic retinopathy is a complication of diabetes. The length of time a patient has diabetes will determine the likelihood of developing diabetic retinopathy. Over 40 percent of patients in the United States, diagnosed with diabetes, have a form of diabetic retinopathy. Diabetic retinopathy is the most common diabetic eye complication and a leading cause of blindness in American adults.
Diabetic retinopathy causes the blood vessels that supply nourishment to the retina, the light-sensitive lining in the back of the eye where vision is focused, to weaken. These weakened vessels can leak, swell or develop thin branches, causing a loss of vision.
Symptoms of Diabetic Retinopathy
Early stages of diabetic retinopathy usually do not show symptoms. Treatment is not always required. Patients need to monitor their blood sugar level to prevent the disease from progressing. If the disease does progress, prompt treatment will be necessary to preserve your vision.
Patients who develop diabetic retinopathy may not notice any changes to their vision at first. In its earliest stages, this condition causes tiny areas of swelling in the small blood vessels of the retina.
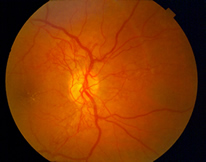
Diabetic NVD
Symptoms of diabetic retinopathy may include the following:
- Vision that may be blurry or doubled
- Flashing lights
- Blank spots
- Dark floaters or spots in the vision
- Pain or pressure in either or both eyes
- Problems with peripheral vision
- Severe vision loss or blindness
In its advanced stages, diabetic retinopathy can cause blurred or cloudy vision, floaters and blind spots and, eventually, blindness. This damage is irreversible.
During any stage of diabetic retinopathy a condition known as macular edema can develop. Macular edema is the buildup of fluid in the macula, the light-sensitive part of the retina that allows us to see objects with great detail. As the macula swells vision becomes blurred. About half of the people with proliferative retinopathy are diagnosed with macular edema.
Diagnostic Testing for Diabetic Retinopathy
After a thorough medical examination of the eyes, some of the following diagnostic tests will be conducted to confirm diagnosis:
- Visual acuity test
- Dilated eye examination
- Tonometry test
- Retinal exam
- Fluorescein/Indocyanine Green angiography
- Optical Coherence Tomography
Treatment of Diabetic Retinopathy
Other than controlling blood pressure, blood cholesterol and the levels of blood sugar, treatment is not needed during the early stages of diabetic retinopathy. The next stage, proliferative diabetic retinopathy is treated with a laser surgery procedure known as scatter laser treatment. During the procedure the abnormal blood vessels are ablated causing them to shrink. This procedure works best once the blood vessels begin to bleed. The procedure in performed in the office.
Severe bleeding that involves the vitreous and may be associated with a retinal detachment may need to surgically corrected with a vitrectomy procedure. The procedure is performed in the operating room using a surgical microscope. The latest advance in that area is being able to perform the procedure with microscopic incisions that do not require sutures. (Micro-incissional or "sutureless" Vitrectomy)
Treatment for macular edema which can be a complication that may occur in any stage of diabetic retinopathy usually includes a laser procedure called focal laser treatment. During this procedure, small laser shots are placed in the areas of retinal leakage around the macula to prevent leakage from occurring and reduce the amount of fluid in the retina. This helps reduce the risk of vision loss and may improve lost vision in a small number of cases. Focal laser treatment is performed in the doctor's office and is completed in one session.
If the macular edema involves the center of the vision, novel anti-VEGF medications can be injected into the vitreous and patients can experience visual improvement. This procedure is also performed under topical anesthesia in the office setting.
Reducing the Risks of Developing Diabetic Retinopathy
Patients with diabetes need to have an annual comprehensive dilated eye exam. The length of time a patient has diabetes will determine the likelihood of developing diabetic retinopathy. Over 40 percent of patients in the United States, diagnosed with diabetes, have a form of diabetic retinopathy.
The risks of developing diabetic eye disease can be minimized by:
- Monitoring changes in vision
- Keeping A1C levels under 7%
- Monitoring and managing blood pressure levels
- Eating a healthy diet
- Participating in a regular exercise routine
- Monitoring and managing cholesterol levels